By Brianna Abbott
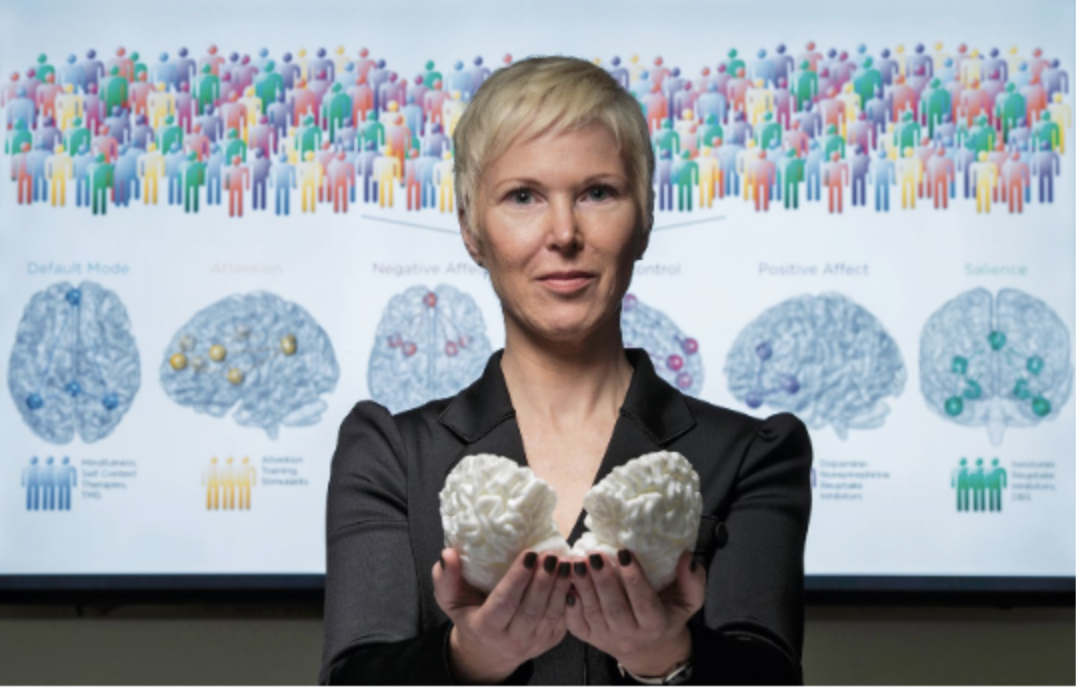
In June 2006, Leanne Williams embarked upon a decade-long study by asking people with panic disorder, post-traumatic stress disorder and clinical depression whether she could record the electrical activity in their brains. She had always wondered how the brain behaved differently in various cognitive illnesses. Over the years, she and her team collected data from 420 people using a technique called electroencephalography, or EEG, to record brain waves. What emerged shocked her. Even among the individuals in the study who shared the same diagnoses, their brain recordings revealed wildly different EEG patterns. Interestingly, the patient symptom data they collected beyond the EEG recordings also suggested that traditional psychiatric diagnoses didn't account for the variability within the illnesses. For example, one patient with depression would complain that they couldn’t stay awake, while another with the same diagnosis had trouble sleeping. Williams could see the diversityin symptoms within the patient groups. “When you're interacting with hundreds of people, the variability really stands out,” says Williams, now a psychiatric researcher at Stanford University in California.
Williams and her team wanted to find a pattern to make sense of the data. But there were too many lists of symptoms and scans to compare and contrast. So Williams decided to turn to an emerging technical tool to make this analysis possible. The team used a form of artificial intelligence called machine learning that can pick out similarities and differences among massive amounts of data to find patterns.
Once Williams and her colleagues had collected enough recordings, they fed the brain scan and symptom data into the machine learning algorithm. Although the study included patients with one of three diagnoses, the algorithm instead fit the patients into six groups, each group with ts own distinct patterns of symptoms: tension, anxious arousal, general anxiety, hopelessness, sadness and calm. These symptom groups comprised traits that repeatedly appeared together. Participants who showed a pattern of ‘general anxiety’, for example, reported symptoms such as breathing difficulty and trembling hands. The EEG recordings further bolstered the idea of these six particular clusterings of symptoms, Each set of symptoms had its own unique pattern of brain waves, according to the machine learning algorithm.
All of this, Williams says, undermines the classic diagnostic labels used in psychiatry. “I was stunned to see just how little the new subtypes fit into the classic diagnostic categories,” she says. “Machine learning defines a whole new kind of subtyping of mental illness.” Williams is laying the groundwork to expand on this idea. In March of last year, she spearheaded the opening of Stanford’s Center for Precision Mental Health and Wellness, which combines traditional mental healthcare with these new disease subtypes based on machine learning.
Psychiatrists have typically relied on patient-reported symptoms, questionnaires and educated guesswork to diagnose the people who come see them. But psychiatry is moving beyond these techniques to tease out biological connections within the brain that were simply unknowable before. Rather than seeing one-size-fits-all diagnoses, researchers are noticing patterns of brain activity that correlate with individual symptoms and point to subgroups of diseases. Researchers hope to home in on what makes each patient’s case unique, perhaps even making more informed prescribing decisions. “Psychiatry is a really appealing and exciting field right now,” says Conor Liston, a neuroscientist at Weill Cornell Medicine in New York. “It’s being transformed by technologies that are enabling us to ask questions that would have seemed like science fiction not so long ago.”
Emerging Subtypes
Psychiatrists currently diagnose their patients using the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which classifies patients into categories on the basis of reported and observable symptoms. But the resulting diagnostic categories, such as anxiety or depression, sometimes fail to capture the complexity of mental illness. Moreover, patients don’t often have only one diagnosis: of the nearly 45 million adults in the US living with mental illness during any given year, roughly 45% have two separate psychiatric diagnoses. Treatment is often a guessing game of trial and error with drug options that have essentially remained stagnant for decades.
In recent years, supercomputer technology has gained greater storage capacity and faster analytic techniques, which make it an appealing tool to neuroscientists drowning in data. Brain imaging machines, meanwhile, have improved resolution. With machine learning, each additional patient profile teaches the algorithm a little bit more about the dataset, making the resulting patterns clearer and more precise. “Teasing out the intricacies of the brain is something that machine learning techniques are perfectly suited for,” says Eric Oermann, a neurosurgeon at Mount Sinai Hospital in New York. “Machine learning is going to increasingly be the go-to technique.”
Theodore Satterthwaite, a psychiatric researcher at the University of Pennsylvania in Philadelphia, and his team used a machine learning algorithm to analyze functional magnetic resonance imaging fMRI) scans, which track blood flow in the brain as a proxy for cognitive connectivity2. The algorithm compared the fMRI scans of 663 adolescents who were being tracked and assessed for symptoms of psychiatric symptoms as part of a study seeking to understand the development of common mental disorders. The scientists sought to find out whether any brain connectivity patterns were unique to those with a history of mental illnesses such as depression and obsessive–compulsive disorder. The algorithm crunched data from 14 different psychiatric conditions and found that individuals could fall into one of four symptom groups: those with strong emotions, hallucinations, fear or physical behaviors. Whereas in Williams’ study the symptom groups mapped to EEG recordings, in Satterhwaite’s study the symptom groups they found correlated to patterns of brain connectivity picked up by fMRI rather than correlating to diagnoses.
Similarly, in a study run by Liston at Weill Cornell Medicine, scientists used machine learning to analyze more than 1,000 fMRI scans of patients with major depressive disorder and healthy controls3,4. Liston and his team saw four unique sets of brain connectivity within the overarching single diagnosis of depression. Each pattern, or ‘subtype’, had its own set of depression-related symptoms: moderate anxiety and insomnia, severe anxiety and insomnia, fatigue or hopelessness. Many anxiety patients had similar brain connectivity patterns to the patients with depression who also experienced symptoms of anxiety. Liston speculates that those patients most likely had the same biological problem despite having different diagnoses. He says this makes sense because those with anxiety and depression sometimes benefit from the same medications.
Through years of trial and error, psychiatrists know that similar drug treatments sometimes work for people with different diagnoses. Even so, matching up patients to the right treatment can take months. If clinicians could instead prescribe medication on the basis of underlying brain activity, they could potentially provide more specific and effective treatment sooner. “What we hope is that maybe this approach will provide a means or at least a starting point for identifying which patients might be most likely to respond to particular treatments,” Liston says.
New diagnostics
With this new mix of machine learning and mental illness as a jumping-off point, researchers eventually want to be able to include machine learning and the biological knowledge it provides as a diagnostic tool. The potential tools wouldn’t be responsible for diagnosis. We don’t need a brain scan to tell a patient that they have major depressive disorder, but the biological groups uncovered by machine learning could assist psychiatrists in choosing the best treatment plan or help researchers develop new treatments targeted for specific brain activity. “Even if 1% of the promise of this stuff was realized and translated into patient care, that would be a massive advance for psychiatry,” Satterthwaite says. “That would get us a little out of the dark ages.”

For now, researchers are still stringing together the various connections between brain activity, reported symptoms and patient care. Researchers are unsure whether the models they’ve discovered with machine learning techniques in their individual studies will translate more widely. And it’s possible that the algorithms they have created might not work with brain scanning techniques universally.
Even though there’s a lot left to unravel, researchers, including Williams, believe that we’ll eventually get to a personalized and more targeted treatment plan for mental health. “We could make the diagnosis in the future in a different way,” she says. “These diagnoses will be based on a specific set of symptoms that doesn’t necessarily respect the boundaries of diagnoses but does respect biology.”