Unraveling Timothy Syndrome: the new science of human brain development
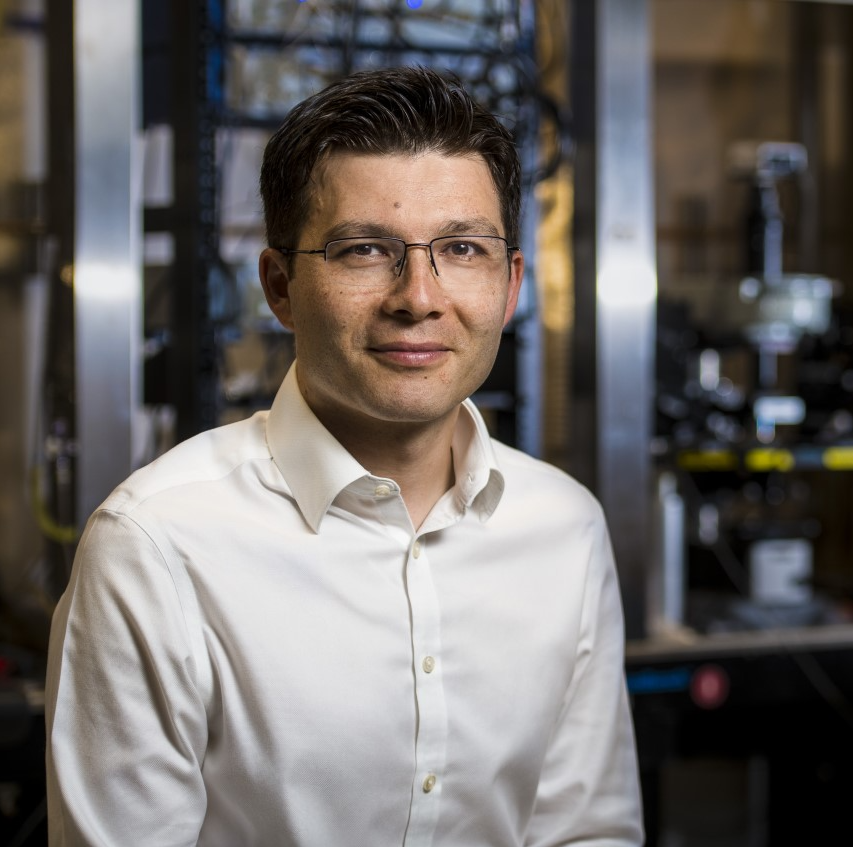
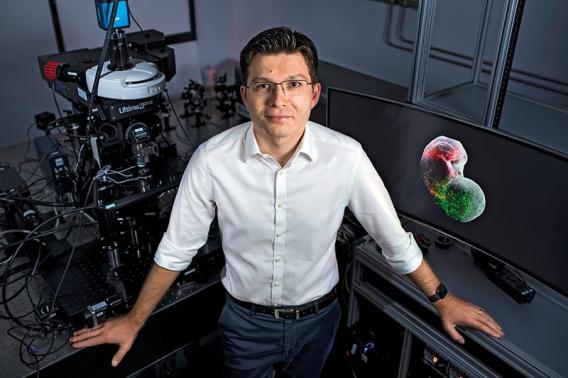
Sergiu Pasca, a professor of psychiatry and behavioral sciences at Stanford Medicine, has developed groundbreaking technologies to grow human brain tissue in the lab, creating organoids and assembloids that model brain disorders like autism and schizophrenia.
This week on the show, Pasca and host Nicholas Weiler discuss the process of turning skin cells into embryo-like stem cells and then into functional brain cells that can live and develop for over two years. Pasca describes his innovative work transplanting these brain organoids into rat brains, a major step toward understanding complex neurological conditions. They also explore potential treatments for Timothy syndrome, a rare genetic disorder.
Join us for fascinating glimpse into the future of developmental neuroscience and learn about the potential for new therapies for our remarkable self-assembling brains.
SUBSCRIBE on Apple Podcasts, Spotify, Amazon Music and more.
Learn more
- Brain organoids and assembloids are new models for elucidating, treating neurodevelopmental disorders | News Center | Stanford Medicine
- Impact of genes linked to neurodevelopmental diseases found | News Center | Stanford Medicine
- Scientists discover how dozens of genes may contribute to autism - The Washington Post
- Study suggests approach for treating rare disorder | National Institutes of Health (NIH)
- How lab-grown brain cells can now help us understand brain disorders (NPR)
Episode Credits
This episode was produced by Michael Osborne at 14th Street Studios, with production assistance by Morgan Honaker. Our logo is by Aimee Garza. The show is hosted by Nicholas Weiler at Stanford's Wu Tsai Neurosciences Institute.
If you're enjoying our show, please take a moment to give us a review on your podcast app of choice and share this episode with your friends. That's how we grow as a show and bring the stories of the frontiers of neuroscience to a wider audience. You can also send us an email at neuronspodcast@stanford.edu.
Episode Transcript
Nicholas Weiler:
Welcome back. This is From Our Neurons to Yours from the Wu Tsai Neurosciences Institute at Stanford University. I'm your host, Nicholas Weiler.
I am very excited for today's episode, but bear with me for just a moment while I set this up. We're back this week with another conversation featuring Sergiu Pasca. He's a professor of psychiatry and behavioral sciences at Stanford University. And we talked with him last year about a remarkable set of technologies his team has developed for growing human brain tissue in the lab. Their goal is to model disorders of brain development like autism and schizophrenia. It was a fascinating conversation. I highly recommend you take a listen. To briefly summarize, and this still feels like science fiction to me, Pasca's team starts with skin cells from a healthy individual or from someone with a developmental brain disorder. They can then use chemical cues to turn back the clock on those cells and turn them into embryonic stem cells. These can be chemically reprogrammed to develop into neurons and other brain cells.
This part is actually not so new. This is a big area in developmental neuroscience. Lots of researchers are doing this much. What Pasca and his team have done that is new is even more incredible. They've figured out how to get these reprogrammed human neurons to stay alive for as long as two years in laboratory dishes. This allows the cells time to follow their genetic programming to self-assemble into tiny models of human brain tissue called organoids. His team can program these organoids to develop in the lab, so they approximate different regions of the brain. They've discovered that if they put these different regional organoids together, they will automatically start linking up as they do in a real developing brain, creating models of brain networks that Pasca calls assembloids. When we spoke to Pasca last year, he told us about the next step his team has taken, which was to transplant human brain organoids into the brains of laboratory rat pups, where they integrate into the animal's brain as it develops.
Now, maybe this all sounds like mad science, but there's a very specific and important reason that Pasca and his team are doing all this. It is very hard to observe the development of the human brain in real time. And what this means is that we don't fully understand what controls brain development and why some people's brain circuits don't develop properly leading to devastating neurological defects. By creating the first viable laboratory models of the developing human brain, Pasca can now, for the first time, test mechanistically how specific genes or environmental factors affect the assembly of neurocircuits. Earlier this year, Pasca and his team use these tools to demonstrate a potential first-ever therapy for Timothy syndrome, which is a rare disorder linked to autism. Now, Timothy syndrome is a very interesting and deliberate choice for these experiments, and that's where we started our conversation.
Sergiu Pasca:
Timothy syndrome is a rare genetic disorder that affects the brain but also the heart. It's caused by a single letter change in the entire genome that essentially causes devastating effects on the product of that gene, which is a calcium channel, essentially a protein that sits in the membrane of excitable cells, brain cells, heart cells, and then essentially lets calcium inside the cell. So, it plays a really key role, this calcium channel in essentially communicating to the cell incoming signals from other cells around it.
Nicholas Weiler:
So, basically calcium channels are just a cellular communication channel that gives the cell signals about what's going on outside.
Sergiu Pasca:
Right. In a way, it kind of like translates electrical signals into chemical signals inside the cells. These are really key proteins, and this disorder was described 20 years ago. And all we knew about it at the time, was that it was affecting the calcium channel, that it was creating a very severe multi-system disorder that was characterized by a very high prevalence of autism. It remains one of the most penitent forms of autism.
Nicholas Weiler:
Which means if you have this gene, you probably will have autism.
Sergiu Pasca:
You're very likely. You're up to 80% likely to have it, which is more than almost all genetic disorders that we know of. But the patients also have epilepsy and intellectual disability. And now that we follow some of the patients for longer periods of time, we know that some of them actually develop schizophrenia as well when they're older. But generally, the patients will present very early on with the heart abnormality.
Nicholas Weiler:
Well, because calcium channels are also critical for the heart cells, right?
Sergiu Pasca:
Absolutely. And so, most of these patients would used to die because of the heart problem. But then actually you can put a pacemaker, brings the heart back on track. And generally patients do pretty well with that pacemaker. But then of course, there's nothing that you can do about the brain. And as this patient developed, they start showing some of the psychiatric symptoms which are really severe and prominent in this condition. Now, this condition, as I was mentioning, is rare. You could say it's ultra-rare.
Nicholas Weiler:
Yeah, I read there were about 70 cases diagnosed in the world, something like that?
Sergiu Pasca:
Yeah, maybe there are like 70. We know of about 40 or 50. And really over the past few years, we went on a systematic search. I've been traveling around the world, both in Asia as well as in Europe, to try to find all the patients. And so, that has actually been taking a lot of time, I must say. It's been really difficult to find the patients.
Nicholas Weiler:
Yeah, I definitely want to come back to that. Hopefully some people listening to this podcast may be able to help in that effort. So, one thing I wanted to ask, and maybe this is where you were going, is obviously we want to help everyone who has a neurological disorder. But I could imagine people wondering, if you only have 40 patients, why are you devoting so much effort? Why is this such a focus for you?
Sergiu Pasca:
You think about psychiatric disorders and neurological disorders, I mean they're really, really hard problem. How does psychosis really arise at the level of networks in the brain? I mean, it's still really, to a large extent, a mystery. Why are so many humans in general affected by psychiatric disorders? A problem of this magnitude has to be cracked somehow. And if you look at all the other branches of medicine and how they've made systematic progress, and just to make it clear, psychiatry is really behind all the other branches of medicine. But if you were to look at other branches of medicine and how when they made progress, you very often will notice that that happened with very rare diseases quite often. So, if you think for instance, think about the cholesterol. Like high levels of cholesterol, a high risk factor for many cardiovascular disorders, it's a rather common problem that's present in a large fraction of the population.
And yet we discover some of the first drugs that tackle this, not in the common population, but actually in a few families, in one family in particular, that had incredibly high level of cholesterol. So, almost like an extreme case. And once we understood what the mutation, where the mutation was in that family, which turned out to be in one of these proteins that essentially processes cholesterol, then you would have a target for some of these drugs. So, very often some of these rare disorders are almost like Rosetta Stones for the other more common disorders. And so, the question is, of course, for psychiatry, what is going to be our Rosetta Stone? How are we going to crack open some of the mysteries of the psychiatric disorders? And you do need that entry point. And that is actually one of the reasons why we picked Timothy syndrome very early on.
Nicholas Weiler:
And the disorder may be extremely rare, but as you said, it's a single letter change in the genome. It affects one gene and one protein. And so, maybe it's solvable. Maybe it's something you can actually understand as opposed to all these other psychiatric disorders that are probably caused by myriad factors, genetic, environmental, and so on.
Sergiu Pasca:
Exactly. And one point, which I think it's important about this, is that in early days, Timothy syndrome was one of the only disorders that was affecting this channel, although this is a huge channel. So, it was a peculiar choice if you think about even studying it when there are so many more common disorders. And yet in subsequent years, especially in the last decade, this channel, which is abbreviated CACNA1C, so this channel actually is now on top of the list of associations with many of the psychiatric disorders.
Nicholas Weiler:
Interesting.
Sergiu Pasca:
So, it's very strongly associated with schizophrenia, with bipolar disorder, with depression. Now of course, it's not the mutation that causes Timothy syndrome, which is an extreme example, but there are actually common variants that all of us are actually carrying and some rare variants that are very associated. So, it does point out that the skeleton channel is a key component, I mean a hub in the molecular machinery behind psychiatric disorders. So, understanding of Timothy syndrome is an extreme example, may give us insights into how perhaps to tackle other conditions as well.
Nicholas Weiler:
Yeah. Well, I think at this point, maybe getting into some of the details about what you have learned about how this mutation that modifies this calcium channel leads to Timothy syndrome would help us understand sort of the process of, okay, now we've got this rare disorder. We know that it affects a particular calcium channel. How does that get us to understanding how it affects the brain and how does that get us to treatment? So, my understanding is that what you've discovered is that this involves interneurons, which are a type of neuron in the brain that helps lower or shut down activity in neural circuits, and how they migrate to where they're supposed to be in the brain. Could you walk us through how you discovered that?
Sergiu Pasca:
Sure. I mean, to a large extent, this has been a 15-year journey of understanding actually Timothy syndrome. We started with very simple experiments early 2009. And think about this, we were like early days when cell reprogramming was discovered. So, Shinya Yamanaka made his groundbreaking discovery showing that you could take skin cells and turn them into stem cells. And I was finishing my clinical training at that time. I thought, wow, this is the most amazing thing that you could actually do to study psychiatric disorders. And of course, I was naive thinking that would not take that long time to actually do.
Nicholas Weiler:
Right. Easy.
Sergiu Pasca:
And came to Stanford. And little did I know at that time how much skepticism there actually was about this approach because people would say, "Oh, you're going to take the skin cells from patients. You're going to reprogram them, and then you're going to differentiate, and that process is going to be long. The phenotypes are going to be gone, so any abnormalities are going to disappear."
Nicholas Weiler:
Right? You're erasing the mature identity of the cell. You're probably erasing the disorder as well.
Sergiu Pasca:
Right. And my expertise was autism spectrum disorders. I was interested in modeling autism. How do you even know that you succeeded modeling autism in a dish when there was no molecular cell or signature of that disease? So, we needed a disorder where the cellular defective neurons would be somehow predictable, and yet if it was to work, it'll be a good proof of principle. So, Timothy syndrome was a great example because the mutation was in a calcium channel. We know what a calcium channel does. I mean, it lets calcium inside the cell and you can measure that calcium. You can even see it live as it goes inside the cell. And it was predicted at that time that the mutation that causes Timothy syndrome, it's what we call a gain-of-function mutation. Meaning that it essentially makes the calcium channel overactive. It stays open for slightly longer, so more calcium should get inside the cells.
So, when I came to Stanford 15 years ago, the first experiments that I set out to do were exactly that, trying to make neurons from patients with Timothy syndrome. We had two patients that we recruited at the time. Made IPS cells, or induced pluripotent stem cells, from their skin cells. And then I started differentiating them in a dish into early neurons. So, they were just at the bottom of a dish, like very simple neurons, very early born neurons. But then you could actually put a calcium dye inside those cells and watch under the microscope as calcium goes up and down in the cells, primarily because of this calcium channel. And I remember that still very vividly, that experiment. It was like July of 2009, when one afternoon I did that critical experiment. And I saw literally, and you could actually see it by eye, I could literally see the calcium going up and staying for much, much longer in Timothy syndrome cells.
Nicholas Weiler:
And it really demonstrated that the naysayers, at least in this case were wrong. That you were able to take those skin cells from patients turn back the clock to make them stem cells and then guide them to become neurons again with chemical cues. And the calcium channels are not working properly, just as you expected. So, your platform for studying Timothy syndrome is there. It's working. It strikes me that your work on the disorder is very closely linked to your development of brain organoids and assembloids. In a sense, you were developing those things to solve problems in studying this particular disorder. Can you tell us how those models allowed you to make breakthroughs in understanding what this calcium channel does in Timothy syndrome brains?
Sergiu Pasca:
Sure. Essentially, it turns out to be more complicated than we ever thought because we were making these neurons. But very soon after I realized, oh, well, they're at the bottom of a dish, so the cultures would die after about a hundred days. This patients developed the psychiatric symptoms so much later. How are we going to keep those cells for longer? And so, we moved them to low attachment plates and we realized that we could keep them now for hundreds, actually for more than a thousand days in a dish.
Nicholas Weiler:
Because they're floating in these little balls?
Sergiu Pasca:
Because they're floating and you don't have to plate and replay them. And even at that time, people were saying that cells can simply not be kept in cell culture for too long, and that corticogenesis or the development of the cortex is actually stalled in vitro, so you can't go too far. I was convinced that it was just a matter of time. If we give it time and we can keep them alive, they will develop. And indeed that was the case. Then of course, very soon after we realize, well, we're only making one single brain region. And even if it is about the cortex, they're both excitatory and inhibitory neurons, this patient have epilepsy. Could it be that there is an abnormal interaction between these key cell types in the cortex?
So, then we introduced the first assembloids, where we put two regions of the nervous system and show for the first time that you can actually see these interneurons, these GABAergic inhibitory cells move towards the cortex. And it turns out that Timothy syndrome have a very prominent defect in this. They move in a very peculiar way. And then we spend, I think four or five years figuring out the precise molecular mechanism for that. And at one point, after about, I would say maybe 10 to 12 years of working on Timothy syndrome, we just started getting such a good understanding of the disorder at multiple levels, at the molecular, cellular and even early circuit level, that the therapeutic opportunity just appear naturally.
Nicholas Weiler:
So, I want to move on to this new paper where you've shown remarkable ability to reverse these defects in Timothy syndrome. Before we get into that, I just want to make sure that we understand exactly what the defects are. So, you mentioned that these inhibitory neurons are moving wrong, and I think it may be surprising for listeners that neurons move at all. So, it's a normal part of brain development that the interneurons are born in one part of the brain and they migrate. They hop along or crawl along all throughout the cortex, the outer part of the brain. And so, if I'm understanding correctly, what you discovered was that because of this calcium channel problem in Timothy syndrome, the inhibitory neurons don't move right, and so they're not getting where they're supposed to go?
Sergiu Pasca:
Yeah. Yeah, that's one of the phenotypes. But actually there are multiple levels of phenotypes. If you go from the gene level, molecular cellular level. So, one of the first ones is actually the calcium phenotype. So, the calcium defect, there's more calcium going inside the cell. So, the cell has to deal with that, has to pump it out. Then there is another defect that it seems to be independent of the calcium. It has to do with a change in the morphology of the cell in the shape of the cells. So, there is a retraction of dendrites in Timothy syndrome.
Nicholas Weiler:
So, usually, cells have these big elaborate trees of... they're sort of antenna for the cell where they're getting signals. And in Timothy syndrome, they're sort of withered.
Sergiu Pasca:
Exactly. And that we know is independent of the calcium going inside the cell. So, it's kind of like a different defect that we've also described almost 10 years ago. And then there is this migration of these interneurons that are not arriving probably at the right time. They're probably arriving with a delay. And so, you have a combination, and all of those are related to this mutation in the calcium channel. But it turns out that this calcium channel changes a lot over time. So, the gene that produces this calcium channel, it's actually processed over time. And initially, it has a lot of the form that carries the mutation. But later, especially in the adult brain, it has only a fraction. About 25% of the gene has the form that has the mutation.
Nicholas Weiler:
So, cells switch to using a different kind that's not affected by the mutation?
Sergiu Pasca:
Exactly. It just does not include the mutation. So, it's another form of the channel that uses an alternative part of the gene, an equivalent part of the gene that does not have the mutation.
Nicholas Weiler:
Interesting. So, it sounds like you almost need to just give the patients time and in that period where their brain cells are using the defective form of the calcium channel.
Sergiu Pasca:
So, that's what we're discovering actually now. And it's still anecdotic and it's not clear, but it seems that some of the patients that are on a pacemaker for the heart, as they're reaching seven or eight years of age, they don't need the pacemaker as much as before. And so, it could be that that is related to the fact that the change has happened also in the heart. So, they now have the other form of the gene that is good. The problem is that for the brain, having that form of the channel for such a long time, could be causing irreparable damage. Yeah, we do need to intervene early. So, essentially, our strategy for developing this therapeutic was exactly targeted towards that.
We thought, let's just help the channel switch to the four that all of us have later in life, and that form won't carry the mutation at all. It's essentially interfering with the splicing, with the processing of this channel. And this is done with tiny pieces of DNA that we've actually screened every five nucleotides until we found one that you literally add to the cells. It gets inside the cells, there's no virus, nothing else. It literally gets shown inside the cells. It goes, and as the gene is processed, it interferes with it and helps the cell decide to take the other isoform that they will have later.
And it works like a dream. Literally within hours, within a day or so, you can see that the cells have already switched to the other isoform. Then within a couple of days, the protein will be changed, maybe two a week. And then what we've discovered is that we can literally rescue almost every single defect that we've described in human neurons over the past 15 years.
Nicholas Weiler:
Wow.
Sergiu Pasca:
So, you add it to the cells, you look at the calcium, the calcium is now abnormal, there's more calcium. You add this a piece of tiny DNA, like 20 nucleotides or so, you add it to the cells, it gets in, you come like three, four days later, the calcium defect is gone. You look at the calcium and the excitability, you add it, that is reversed. You actually make four brain assembloids where cells are migrating onto the other side. You let them migrate for a week, you end the antisense, and then it just helps the cells get to their destination.
Of course, the challenge at that time for us was, okay, well, we have this great system. There is an animal model for the disease, but it does not recapitulate many of the features of the disease. So, now they're in a puzzling situation. You have a potential therapeutic that works in vitro in a dish, but you have no proof that it works in a living organism. And we've learned in the last few years that that is actually critical. Not just because sometimes some of this simply don't work in vivo context, but also because sometimes you have unanticipated side effects. And there have been a few cases where some of this antisense oligos have literally been lethal to some of the patients.
Nicholas Weiler:
And the antisense oligos, that's the term for these tiny pieces of DNA that cause the cell to switch which version of the calcium channel is using. So, those sometimes have unintended consequences. So, you really needed a way to go beyond the lab dish and show how this would affect actual brain development.
Sergiu Pasca:
But the problem is that we don't have an animal model for this disease that works. So, then actually we turned to a system that we've developed several years ago, kind of like independently of this approach, which has to do with growing some of this cortical organoids inside an animal's brain. We do this through transplantation, putting some of those cortical organoids early in the developing rat brain so that they integrate. And you essentially build about a third of a rat hemisphere to be made out of human cells in a very predictable position in the somatosensory cortex. And so, we did exactly that.
We transplanted now patient cells from actual Timothy syndrome patients inside the rats. You waited for like nine to 10 months, and then as you were doing a patient where, by the way, this drug has to be injected inside the nervous system intrathecally, we actually injected the drug into the rat, waited for about a week to two weeks, and then look inside the graft in human neurons. So, the idea is that you treat the rat, but you look at the effect on human patient cells. And then as we've seen before in vitro, now suddenly we saw the calcium defect is reversed. Patients, as I've told you before, have this retraction of dendrites. Their processes are retracted. You literally look after 10 days and they're back. They're exact like the control cells. So, you even restore some of this morphological defect. And to the extent that we've tested so far in rats, we didn't find any unanticipated side effects.
Nicholas Weiler:
I find this just so incredible the way this technology has developed. If you think about the whole chain of events now that has to happen to make this work. You have a skin cell from a patient with Timothy syndrome. You can cause that skin cell to become an embryonic stem cell and then reprogram it to become a neuron. And then grow it in a lab dish as this little organoid ball floating in the solution. And it starts to look just like a developing human brain in many important ways. You can even create multiple ones that go together and the cells will start migrating. They'll start interacting in the way they're supposed to. And then you can implant just after the rat is born, a major part of the rat brain is now made up of these human neurons derived from the patient. So, now you've got a rat with a large portion of its brain made up of patient-derived human cells, and now you can show that this drug really works on human cells in an actual developing organism to revert them back to seemingly normal appearance and function. It's truly incredible.
Sergiu Pasca:
Yeah, thank you. It's been quite a journey. And I'm starting to think more and more, and I've been making this more clear even in some of the papers, that for understanding psychiatric disorders or for modeling them, we will need a multi-level approach. So, we will need to look at multiple level and it will need to involve some sort of circuit level readout as well. And so, I think some of this transplantation approaches are precisely going to help in that regard.
Nicholas Weiler:
So, I was excited to read that very recently, the FDA also opened the door to a faster clinical trial process for situations like this where you can't really do the normal set of pre-clinical experiments. You're currently looking for patients and developing plans to run a clinical trial for this drug that you've developed and tested with your organoid models and your transplantation models. Obviously this is a first step. But it illustrates so nicely the hope for understanding and treating this neurodevelopmental disorder and hopefully, other neurodevelopmental disorders from autism spectrum disorders, to bipolar and schizophrenia. Could you comment a little bit on how you see this leading to a new way of doing neurodevelopmental clinical research?
Sergiu Pasca:
Well, I think first of all, it's true. We're thinking very deeply about the next steps in terms of clinical translation. And so, I've been putting together a translational neuroscience group here at Stanford, where we have clinicians as well as researchers, thinking very deeply about how exactly we're going to deploy some of this therapeutics. And by the way, Timothy syndrome is the first one that is coming, but we have several others that are at various stages of development. And then there are all kinds of challenges because again, we don't have some of the animal models. And it's good that the FDA has opened up the door of doing that without, but at the same time, we have a huge responsibility of making sure that these drugs are actually safe for the patient.
So, we're thinking very carefully about the next step in terms of safety. For instance, do we need to inject in non-human primates to make sure that there are no other unanticipated side effects before we go into these patients? Who, by the way, are also very sick, so they have a lot of comorbidities and other conditions. There are some amazing advantages in a way with Timothy syndrome versus other conditions. And one of them relates to how early is too late to intervene for a neurodevelopmental disorder. Because the brain has already been developing. And most forms of autism get diagnosed by the second or the third year of life. By that time, a lot of damage has already been done.
And the one fundamental question in the field as we're thinking about translation, is how much of that can you actually reverse? Now, with Timothy syndrome, there is actually a unique advantage, so to speak, that this disorder is one of the only forms of autism, it may be the only form of autism, that actually gets diagnosed within the first week of birth. Because this patients will be born, they have syndactyly, so they have webbing of the finger that is not necessarily highly specific, but they'll immediately have the heart abnormality. And even if the pediatrician of the neonatologist has never heard of Timothy syndrome, because it's such a rare condition, they will try to exclude first metabolic and other sources of the heart abnormality, which is a long QT segment. And once they've actually done that, they'll have to send for a genetic panel. And generally the genetic panel will indicate that this is a specific time of long QT syndrome that is also known as Timothy syndrome.
So, we have the opportunity here to actually diagnose within the first couple of weeks of birth. And because this disease is so severe, so it has high penetrance, so it's not like some patients are actually absolutely fine, so you don't want to take a risk of intervening, but actually all the patients that we know of are very, very sick. You can actually intervene early or as early as we can for this disease. So, that is a unique opportunity. And the Timothy syndrome community has actually been very active, and now they are essentially putting together this larger group in preparation, in anticipation for a clinical trial. But I do believe that, I think more broadly, this opens up the possibility. This is, to a large extent, the first disorder that is fully understood or a therapeutic approach is exclusively developed with human stem cell models, starting with 2D to 3D organoids, assembloids, and following transplantation.
So, certainly we're going to have to be very careful about making sure that this approach is overall safe. It hopefully will serve as an example for other conditions and for others to actually do this. And I must say, since we've published this paper in April, so late April, I literally got hundreds of emails from researchers who are even been thinking about similar approaches for some of those disorders. Or actually now thought, okay, we're going to try to do this multi-level approach and including the transplantation approaches. So, there's been a lot of movement in the last few months, which I think it's exciting, and then hopefully will yield something even if it's not for us, for somebody else.
Nicholas Weiler:
Right. Well, Sergiu, thank you so much for coming on the show. Again, I can't wait until our next conversation.
Sergiu Pasca:
Yeah. Thank you so much for having me. Thank you.
Nicholas Weiler:
Thanks again to our guest, Dr. Sergiu Pasca. You can learn more about his work in the show notes.
If you're enjoying the show, please subscribe and share with your friends. It helps us grow as a show and bring more listeners to the Frontiers of Neuroscience. We'd also love to hear from you. Tell us what you love or what you hate in a comment on your favorite podcast platform, or send us an email at neuronspodcast@stanford.edu.
From Our Neurons to Yours is produced by Michael Osborne at 14th Street Studios, with production assistance from Morgan Honecker. Our logo is by Amy Garza. I'm Nicholas Weiler at Stanford's Wu Tsai Neurosciences Institute. We'll see you next time.