Mitochondrial meltdown in Parkinson’s disease: Q & A with neuroscientist Xinnan Wang
Xinnan Wang, MD/PhD, is an assistant professor in Stanford’s Department of Neurosurgery. She is fascinated by the power plants of cells, known as mitochondria.
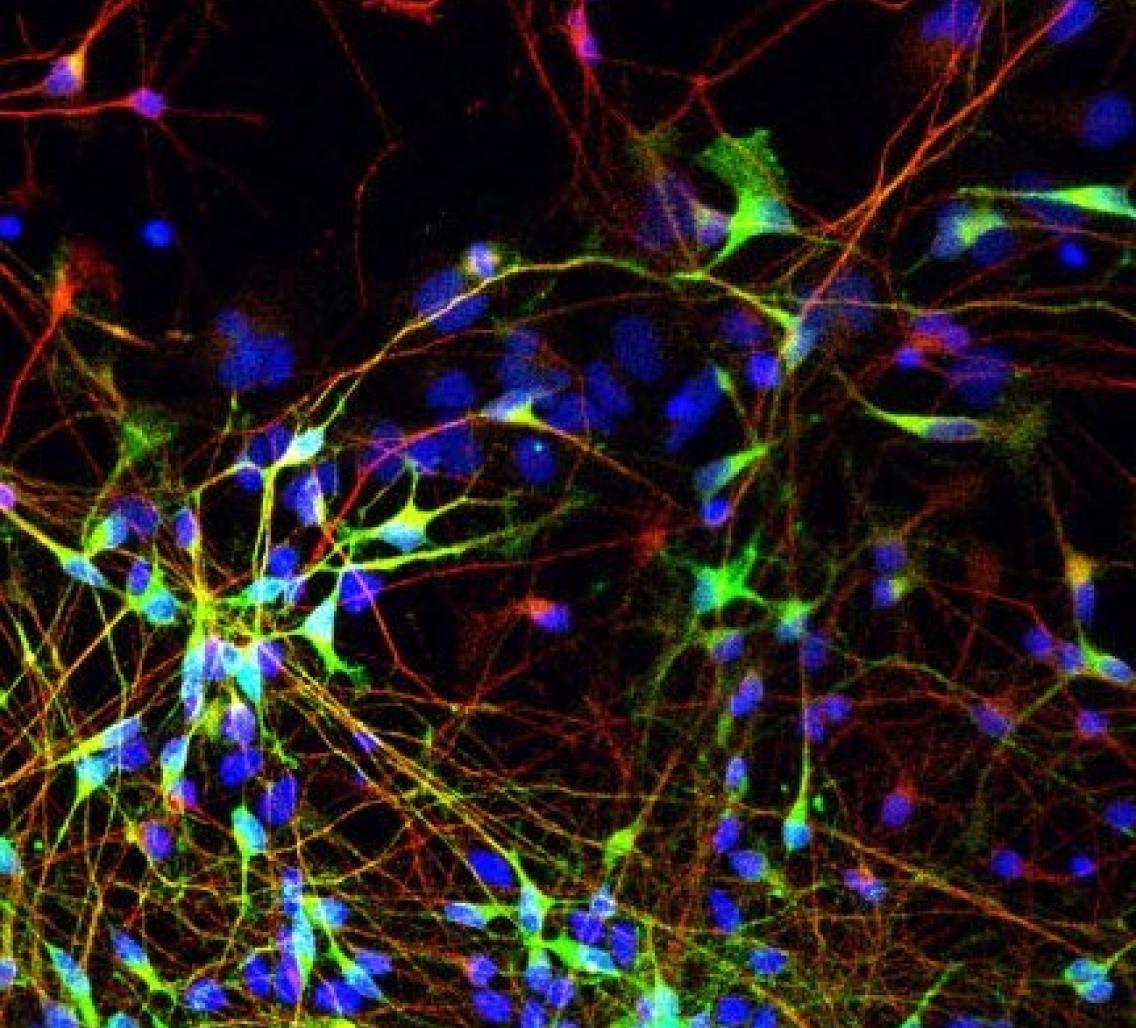
Mitochondria in brain cells (neurons) can undergo “nuclear meltdown”: They stop producing energy and start producing toxins, which if not cleared up quickly will kill the neuron. Wang's lab has recently shown that both familial and sporadic cases of Parkinson’s disease may stem from an inability to clean up these meltdowns. Meredith Course spoke to Dr. Wang about how she got into the field and about recent work published in Cell Stem Cell.
What is the focus of your lab?
My lab studies the movement of mitochondria in neurons, and how its disruption contributes to neurodegeneration.
How did you get interested in mitochondrial movement in neurons initially?
Mitochondria are critical to neuronal health, but the mechanisms underlying how mitochondria move in these cells weren’t really clear when I started in this field as a postdoc. People didn’t understand how mitochondria moved, and people didn’t understand how important it was. For example, at a mitochondria conference in 2008, Bill Saxton [Professor of Molecular, Cell, & Developmental Biology at UCSC] showed a movie of mitochondria moving in axons. The audience of mitochondria researchers was awed and surprised because they had never thought about how mitochondria are able to move. And for neuroscientists, it is a topic that people ignored for years, even though mitochondria have to move around a lot in neurons to provide energy in all the different places it is needed.
In my postdoc lab [Thomas Schwarz, Professor of Neurology and Neurobiology at Harvard Medical School], we contributed significantly to this emerging field. We set up systems for imaging mitochondria in live neurons, and for analyzing and interpreting the results. We began to suspect that mitochondrial transport may play a role in Parkinson’s disease when we discovered that both PINK1 and Parkin—proteins whose mutations cause the disease—regulate a mitochondrial transport protein called Miro. When these proteins aren’t working properly, they can’t regulate Miro, and the result is that damaged mitochondria are not quarantined and removed, and they start producing toxins that hurt the cell. The clear next question was: Is this impairment associated with other Parkinson’s disease mutations? That question formed the foundation our current work.
What did your recent paper in Cell Stem Cell find?
We discovered that this impairment in regulation of Miro may actually underlie both familial (inherited) and sporadic (not inherited, or unknown family tree) forms of Parkinson’s disease. In skin cells and neurons cultured from human patients with both known and unknown Parkinson’s disease mutations, we showed that Miro is consistently mis-regulated. Miro ties the mitochondria to motors that drive the mitochondria around the cell. When mitochondria are damaged, they need to be untied so that they can be stopped and removed from the cell. In Parkinson’s patients’ cells, Miro is stuck to mitochondria, so damaged mitochondria can’t be removed. Damaged mitochondria pile up, causing energy shortfalls and accumulation of toxins, which eventually kill the cell.
A large part of our paper focuses on the fact that we found this impairment in the most common genetic cause of Parkinson’s disease—mutations in a gene called LRRK2. These mutations are found in 1 in 20 familial cases, and 1 in 50 sporadic cases (when the cause can be identified through sequencing). Normally LRRK2 attaches to Miro and removes it from damaged mitochondria, similar to how PINK1 and Parkin remove it. When LRRK2 is mutated, it can’t do this job. We were then able to show that this mechanism is common to all the major familial forms of the disease as well as to sporadic cases tested so far.
Did you expect to find a common nexus of Parkinson’s disease pathology?
To be honest, I was really surprised. I didn’t expect that Miro could link to LRRK2 at all because there was absolutely no connection known, but that’s how science works!
What does this finding mean for Parkinson’s disease patients?
The reason this is significant is that you could use this impairment in Miro removal as a biomarker to diagnose the disease and find people at risk, or identify people at different stages to better develop strategies to treat the disease. Additionally, you could target this nexus to design novel strategies that work for both sporadic and familial cases. Targeting Miro is something we are trying to figure out. So far there are no available drugs that target Miro, so answering that question requires future studies.
What’s next for your lab?
The immediate follow-up work is to study how Miro is impaired in sporadic cases, and to ask how disruption of mitochondrial movement may contribute not just to Parkinson’s disease, but other neurodegenerative diseases. For example, we are also looking at mitochondrial transport in ALS [amyotrophic lateral sclerosis]. We are also trying to understand the basic biology of many disease-causing genes.
Meredith Course is a 5th year neurosciences PhD student in the lab of Xinnan Wang.